When Katie Clow and her research students arrive in a windowless lab at the Ontario Veterinary College, in Guelph, Ontario, on a drizzly late-fall morning, envelopes have piled up on their workbench like a manila snowdrift. They slip on white coats and reach for scissors to start slitting open the padded packets. Each one contains a slip of paper and a small plastic vial or two. The paperwork lists the name of a veterinary clinic somewhere in Canada and the identifying details of someone’s pet: a six-year-old golden retriever in Moncton, a four-year-old tabby in Victoria.
Listen to an audio version of this story
For more audio from The Walrus, subscribe to AMI-audio podcasts on iTunes.
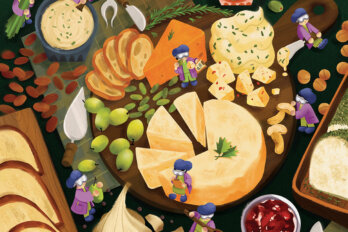
Inside each corresponding vial is a tick—or fifty—plucked from the body of that pet and mailed in for research. With her team, Clow, a professor of veterinary medicine with expertise in epidemiology and ecology, opens the vials and tips the rigid bodies of the arachnids into a petri dish. Unless they’re not dead: after a week or two in the custody of Canada Post, they sometimes emerge and start scurrying across the bench. When alive one tumbles out in front of research assistant Kiera Murison, she snatches apair of tweezers to pluck it up and deposits it into a vial of ethanol, with a whispered apology, swirling it around to bring a prompt demise.
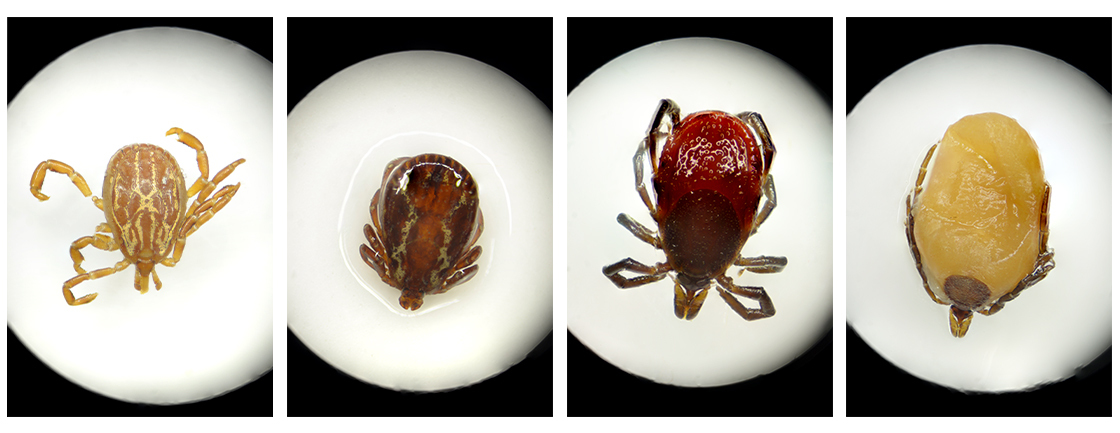
When the ticks are all definitely dead, they are stored in the fridge until Clow, an ebullient thirty-two-year-old whose students call her the Tick Queen, has time to sit down with a box of them. She identifies the ticks quickly, by species and by gender, based partly on the appearance of their hard outer shell, called a scutum, and sometimes by the shape of their protruding mouthparts. Most of the ticks mailed to her Canadian Pet Tick Survey are American dog ticks, Dermacentor variabilis, or blacklegged ticks (also called deer ticks), Ixodes scapularis: those are the two types you are most likely to find on your pet or your tent or your toddler this summer.
Once identified, the ticks go under the knife: with a scalpel blade, Murison slices them to bits. Ticks that were found and removed before they had time for a long feed are smaller than a watermelon seed and nearly as crunchy: they resist the scalpel. But the engorged ticks, the ones that had a hearty blood meal, can be swollen up like a stewed cranberry. Cutting them is more like carving a soggy M&M. “You definitely hear the outer shell breaking,” says Murison, hacking away at a rigid American dog tick so vigorously that her blond ponytail swings back and forth. When the engorged ticks are dissected, they give off a loamy smell from the coagulated blood that has ballooned them to as much as ten times their original size. Clow and her team marinate the chopped ticks in chemical reagents then run them through a process that extracts the dna in the bug hash. There are two main types of genetic material they are looking for in blacklegged ticks: that of Borrelia burgdorferi, the bacteria that causes Lyme disease, and Anaplasma phagocytophilum, the cause of anaplasmosis, which brings fever, vomiting, and in rare cases, can cause respiratory and organ failure. Clow finds B. burgdorferi in about 25 percent of samples; A. phagocytophilum is much more rare, found in just 1 to 2 percent.
Murison shoves aside a heap of envelopes and shakes her head at the pile. “We’re not supposed to be getting this many in October,” she says. There are ticks in all seasons now. Lyme rates are surging because the ticks that spread it—I. scapularis, predominantly—are rapidly expanding their range. Climate change has made much of the most populated part of Canada an ideal habitat for many species of ticks; I. scapularis, which spreads Lyme, in particular, is rapidly expanding its range. In the early 1970s, there was just one known colony of blacklegged ticks in Canada, at Long Point, on the north shore of Lake Erie. By the 2000s, the tick was being found all over southern Ontario, Quebec, Manitoba, and the Atlantic provinces. Today, they’re marching steadily west from Manitoba on their eight tiny legs.
I. scapularis is no bigger than a poppy seed when it does most of its damage, but this particular tick is emerging as an outsize threat. “Their capacity to move into new areas and to take advantage of suitable habitats and warming climates is completely different,” says Robbin Lindsay, a research scientist at the National Microbiology Laboratory in Winnipeg. Lindsay has studied this particular tick extensively in a long career that has made him an internationally recognized expert on vector-borne illnesses. He has been bitten by hundreds of ticks, a couple of which made him hideously ill, and yet, when he speaks of I. scapularis, admiration suffuses his voice. “The sky seems to be the limit for them,” he says. “They are taking over the reins as the number one vector of pathogens to humans. And that’s only changed in the last twenty years.” I. scapularis is “extremely catholic with its taste for blood,” Lindsay says. It will feed on both migrating birds and big mammals that cover wide ranges—helping it expand its territory—and it’s also delighted to encounter a human and her dog. In tick-borne disease literature, the blacklegged tick is almost universally described as “aggressive.”
The knowledge that this tick is proliferating in the most densely populated area of Canada, potentially spreading not just Lyme disease but anaplasmosis and babesiosis, an infection that resembles malaria, is disturbing in ways that it feels as though we have not yet grasped. It will precipitate a significant change in how Canadians view our relationship with our environment. When I asked another tick expert, Nick Ogden, a research scientist at the National Microbiology Lab, how much he worried about ticks, he explained that, since he did much of his research in Africa, where he was thinking about puff adders, typhoid, cholera, malaria, and about a dozen other things that might kill people, ticks figured fairly low on his list.
In Canada, however, the list of ambient things we must fear is not long. Outdoors, it’s grizzlies, rattlesnakes, maybe a rogue cougar if you are massively unlucky, and of course, the cold. Otherwise, it’s icy highways, drunk drivers, and unstable ladders. But we don’t need to worry much about lethal things lurking in our gardens or in the dark corners of our closets. Or, rather, we didn’t need to. Until now.
On a cold grey autumn afternoon, Katie Clow takes me into the woods, an hour’s drive from Guelph, to drag for ticks. She equips me with a white hazmat suit, seals off my ankles with duct tape, and hands me awhite flannel blanket taped to a metre-long stick. Then we set off into the underbrush, dragging the blanket awkwardly over brambles. We pass a few hikers, who take one look at our CSI getups and our blankets and hurry away. Clow and her team of students go dragging every year, and every year they find ticks farther north. “One year you find a couple of ticks,” she says, “and the next year you’re finding half a dozen ticks, and the next year you’re finding ten ticks and Borrelia.”
Where there is Borrelia burgdorferi, there’s a risk of Lyme. The disease causes fever, fatigue, and joint aches, and it is an emerging public health problem. There were 2,025 cases reported to the Public Health Agency of Canada in 2017, the last year for which data is available, but the agency speculates that number is underreported and predicts as many as 10,000 new cases each year in the 2020s. Huge swaths of Ontario, Quebec, Manitoba, New Brunswick, and Nova Scotia are now considered Lyme risk areas. But, at the same time, we’re more aware of Lyme and how to manage it: many people who spend time in areas with ticks know to do a “tick check” after being outside and know that, if you find and remove the bug within twenty-four hours of when it began to feed, you can’t get the Lyme bacteria. While there is no vaccine for Lyme available, the bacteria is treatable with antibiotics. If you don’t find the tick or don’t get the telltale bull’s-eye rash, Lyme can be harder to identify, and you can suffer symptoms for weeks or months until diagnosis. A small subset of those infected report a “chronic” infection, although most scientists reject the idea this could occur; one hypothesis is that the so-called chronic infections are actually coinfections of Lyme and another tick-borne pathogen, such as Anaplasma, for which doctors do not routinely test.
After about an hour in the forest with Clow, I stop for a periodic inspection of my blanket and, right near the top, heading with surprising speed for the handle (and my bare hand) I see—something? “Katie,” I ask, “is this a tick?”
Clow hurries to me, leans in for a look, and lights up like Christmas morning. I have picked up an adult female blacklegged tick, with a black hood on a handsome dark-red scutum. A short while later, Clow finds a tick on her own blanket and is equally pleased: you’d never guess she has encountered 10,000 ticks in her professional life. She identifies it—another I. scapularis—then sets it gently down on a leaf so I can have a good look. The tick immediately scooches to the end of the leaf and begins to wave its front legs back and forth.
“Ooh,” Clow croons. “She’s questing!”
A questing tick waits at the end of a blade of grass or leaf, with its legs outstretched, tracking the changes in heat and CO2 that signal that something biteable is walking by, poised to jump aboard—a sort of arthropod hitchhiking. Watching Clow watch the tick, I recognize the phenomenon that I saw in Robbin Lindsay and every other tick expert I talked to: the admiration for ticks, for their adaptability and ingenuity and complexity.
A tick can live for a few years without feeding. But, like a video game vampire, they need blood—a “blood meal,” as it’s known in the zoology world—to level up and move between stages of the life cycle. They start out as eggs, typically laid in the leaf litter on a forest floor. (But some, like the brown dog tick, will deposit eggs in a convenient crevice in your floor.) The eggs hatch into larvae, with just six legs, usually in late summer, although the seasonal timing varies between ticks. And thus begins the hunt for a host—a reptile, bird, amphibian, or mammal that will provide the blood that will allow them to mature. When the larvae have fed on something small, they drop back to the ground and moult, becoming a nymph. They will overwinter, burrowing under the leaf litter to keep warm. As nymphs, they develop that last set of legs, and at this stage, they can host many pathogens. When the next blood meal happens, typically off a larger creature, they are able to be infected with bacteria or viruses—and to pass them on, when they feed again, as an adult. Nymphal ticks are tiny, and thus much harder to spot and remove, so they’re the ones most likely to get away with making their way inside your trousers and having a long feed. After the nymph moults again to become an adult, it quests its way onto a larger host, such as a dog or a deer or a human. Males and females meet and mate on a host before dropping off; some species lay several thousand eggs in a process that can take weeks. If a female doesn’t find a host to reproduce on in the fall, she burrows back into the leaf litter and waits for spring.

It’s a risky requirement, this need to feed on an exponentially larger and faster-moving host, when you’re a slow-moving creature the size of a sesame seed. And it’s the range of ways that ticks have found to navigate that risk that seems to make the tick people really excited. I asked Nick Ogden, a soft-spoken man from the north of England who emigrated to Quebec after studying Lyme disease at Oxford, why he chose ticks when he was starting out as a veterinary scientist—given that he had his choice of creatures great and small. He started off casually but, in seconds, had revved up into a full-throated praise song:
They’re just amazing, amazing parasites. They are immensely tenacious. You find ticks pretty much everywhere in the world, in a whole lot of different ecological niches to which they have adapted themselves. Their whole biology is fascinating, how they sense hosts around them by being able to smell the CO2 we produce and the other kinds of pheromones that we’re producing. Then there’s their whole feeding thing: everyone thinks it’s like mosquitoes, that they’re just like a syringe, but they’re fascinating! They dig a hole in us, they bury their heads in, and they feed for up to two weeks. The mouthparts of an adult female tick are about the size of a splinter. The first thing that you feel with a splinter is that it hurts. And the first thing that you feel when a mosquito bites you, either it hurts or it stings. But you don’t know the tick is there!
A tick can coat its body in its own saliva, a liquid salty enough to pull moisture from the atmosphere. That is sustenance enough to keep it going for months—or even years—while it’s waiting for a meal. The saliva is produced in glands that can occupy as much as a third of the tick’s body cavity, and when it is time to feed—the most dangerous time in a tick’s life—this liquid is its primary defence mechanism against a host’s immune system. When you stroll by and a questing tick makes the successful leap, it attaches in one of two ways: by transuding a sort of glue to keep its mouth in place, or, as with the blacklegged tick, by poking barbed mouthparts into your flesh. When a tick bites, it begins by secreting enzymes that destroy a circle of flesh and create a tiny puddle of blood, which it begins to suck up. (A tick takes in blood and sends out saliva in alternating cycles.) The tick needs to kill pain so you won’t realize it’s there and flick it off. And it needs to stop your body from mounting the immune response that it would otherwise send against this intruder from the moment its mouthparts pierce your skin. Among the 3,500 proteins identified in the saliva of various ticks, some stop the molecules carrying a pain signal, while others are vasodilators, to get the blood flowing, or anticoagulants, to keep it from clotting. Some proteins stop the histamine response, which would make the bite itch and clear a path for immune cells to reach the site. There are also molecules that inhibit white blood cells. And, because the tick needs to keep feeding for days—keeping your immune system fooled—it changes up the protein composition of its saliva, like a dash into a phone booth for a new disguise.
So there you are, with a tick feeding and passing pathogens into your body after having disarmed your immune system. It’s the ideal situation, Ogden says, for a virus or bacterium looking to fulfill its evolutionary obligation by finding new animals to infect. “If a bug has to get from an arthropod into a host, what a wonderful gateway it is, where the tick’s feeding.”
Ticks like their tissue soft and thin, as Eric Stotts can tell you. Last October, Stotts went on a guys’ weekend to a cabin near Port Mouton, on Nova Scotia’s south shore, a couple of hours from his home, in Halifax. An affable forty-eight-year-old architect, Stotts goes with his buddies every year, and in addition to a lot of eating and drinking, they always take on a project and learn a new skill that someone in the group can teach. Last fall, it was filmmaking, and Stotts spent much of the weekend crouching and lying on the forest floor as he filmed long still shots of the last dark yellow leaves on the trees—aiming for what he called a “kaleidoscopic” nature effect. He thought his film turned out pretty well, and when he was back in his home office on Monday, he was feeling good about things.
Until he went to pee.
And there, on the end of his penis, was something small and black. “I kind of poked at it enough to realize, Okay, it’s definitely attached, it’s not moving,” he says. And that’s when he thought, Tick. He zipped up his pants and headed to the medicine cabinet for tweezers. His wife worries about Lyme disease, so he knew the procedure: he had to make sure he got the whole tick out, including the head and mouthparts now buried in his most sensitive skin. “I had to be a little bit more aggressive than I would have hoped,” he remembers. There was digging. But Stotts is the sort of fellow who likes to find a bright side, even when gouging the end of his penis with a sharp instrument. “In a strange way, I was kind of grateful that it was so obvious, you know, because, had it attached anywhere else, it could have gotten to the point where the transmission of Lyme disease could have happened,” he said. “It picking the most prominent, visible spot ended up being a real advantage for me, actually.”
Using Google, Stotts quickly confirmed that his new companion was I. scapularis. He kept the tick bits and headed to his walk-in clinic, wondering if the tick should be tested for Lyme. He was waiting in an exam room when a nurse came in to ask what ailed him. Stotts decided there was no point in trying to maintain decorum.
“I had a tick on my dick,” he said.
The response was not what he expected.
“Well, that’s the second one I’ve had this week,” the nurse told him. (The other patient had actually had a tick on his scrotum, which Stotts considers far more distressing and invasive than a tick on the penis. He feels sorry for that guy.)
The doctor Stotts saw did not send the tick for testing: at this point, the protocol is to prophylactically treat anyone likely to have been exposed to Lyme disease. Stotts swallowed “horse pill” antibiotics for two weeks and sent an email to all the guys who had been with him that weekend, warning them to do a tick check.
He did not, for the record, attach a tick dick pic.
Even a decade ago, when Stotts started going on those weekends away, there were only a handful of tick populations in Nova Scotia; now, the region south of Halifax is the second biggest source of mail-ins for Clow’s pet tick study, which began last year. But the section of Canada that makes a suitable habitat for ticks—and for I. scapularis in particular—has expanded dramatically over the past twenty years. There is a lot of debate among scientists about why that is, but climate change figures in almost every hypothesis. Of all the environmental factors that affect the size of tick populations, temperature is the most important. Shorter, warmer winters are good for tick life cycles. It’s not that they freeze in winter—they can weather the cold hunkered down in the leaf litter of wooded areas. Rather, when it’s colder, a tick takes longer to quest and is slower to move through each stage of the life cycle—so a greater proportion of them die before the cycle is completed. At the same time, milder winters mean that migratory birds are nesting progressively farther north, transporting ticks with them to establish in new areas. Hardy I. scapularis has proven adaptable to a range of climates, from Florida to Nova Scotia.
Research conducted in the 1980s, when Lyme disease was emerging as a serious public health problem in the US, showed that most of Canada was too cold to have to worry about the blacklegged tick; Ogden found the same thing in the early 2000s. But the research reveals the speed at which the impact of a warming climate has been felt: Ogden and Lindsay contributed to a paper, published in the Journal of Applied Ecology in 2012, predicting that “the proportion of the human population of eastern Canada inhabiting areas with established tick populations [would increase] from 18per cent in 2010 to over 80 per cent by 2020.” And they were right, although Ogden wishes it were otherwise. “It’s gone from a model-based hypothesis to a public health reality in a decade,” he says. Meanwhile, the white-footed mouse, the most important reservoir for the Lyme bacterium, is also expanding its range north. It likes the short winters, too, and breeds more rapidly than it used to.
And then there are other ecological factors, such as forest fragmentation: when urbanization breaks contiguous wooded areas up into patches. You might think that would reduce the amount of wildlife around and thus be bad for ticks, but by condensing the populations of some mammals (such as those mice) while evicting large predators, such as cougars and wolves, that would eat the deer that are a preferred host for adult I. scapularis, it creates a sort of tick food court.“We see every year this creep northward,” Clow says, “where sites that didn’t have ticks the year before are now positive.”
On a September day in 1958, a tow-haired four-year-old named Lincoln Byers was in the barn on his family’s farm, twelve kilometres west of Powassan, Ontario, when his brothers noticed his eyes were acting funny, flicking to the side, and he had a tremor in his arm. His parents took him to see the family doctor, who took one look and urged them to get him to The Hospital for Sick Children, in Toronto, a six-hour drive in those days. When they got there, Lincoln was feverish but with no obvious cause of illness. Two days later, he was fading in and out of consciousness, and monitoring of his brain suggested it was inflamed. On the fourth afternoon, he suddenly stopped breathing and was placed in an iron lung. He died two days later.
His devastated parents gave permission for an autopsy to two physicians, one of whom was Donald McLean, a virologist at the hospital who had been following the case closely. They cultured fragments of Lincoln’s brain and injected the product into mice, which developed signs of acute encephalitis. But, when the samples didn’t come up positive in serology tests for any known encephalitis, McLean and his collaborators realized it was a new virus.The closest comparison they could find was a virus that, in Russia, was transmitted by ticks. So McLean hung up his lab coat, picked up a shotgun, and drove his team to Powassan. They began around the Byers’s farm and worked outward: they killed squirrels, chipmunks, rabbits, and other mammals, and harvested any ticks they found. Back in the lab, they found that some of the animals also activated the blood test they had developed for the new virus. Eventually they concluded that Lincoln, the second youngest of nine children, had likely been bitten by an infected tick while holding dead squirrels his brothers were skinning. McLean and his colleagues also tested the blood of park rangers and others who worked outdoors around Powassan, finding that several of these people carried antibodies to the virus; they expanded their investigation to the blood bank in Sudbury, where they confirmed that a percentage of the population had been exposed.
Newspapers ran alarmed stories after McLean published his research, but Lincoln’s death remained a tragic exception. By 2009, fewer than fifty cases of what came to be called Powassan virus had been reported anywhere. That, Katie Clow says, makes for an interesting epidemiological mystery: the virus is clearly circulating somewhere in the wild, being passed from ticks to mammals and back again, often enough that there are these rare infections—but not a major public health threat.
The discovery of Powassan virus, a vicious form of encephalitis that can cause permanent neurological damage or death, in I. scapularis changes how we have to think about that risk. I. scapularis can pass the virus to its eggs, so its offspring do not have to progress through the life cycle and get infected to become vectors. And, while the public health response to Lyme disease is based on tick-checking—because it will take the tick at least twenty-four hours to pass on the bacteria—this is not the case for Powassan. A tick needs to feed on you for only about fifteen minutes to transmit that virus, explains Nicole Nemeth, a veterinary pathologist and expert on arboviruses, including Powassan, at the University of Georgia. Lyme bacteria live in a tick’s gut, and when the tick starts to feed, the bacteria begin to multiply and make their way through the gut wall and up to the salivary glands, where they are transmitted to the host. But Powassan lives and reproduces in a tick’s salivary glands, so it’s right there, ready to go the moment a tick bites.
Powassan virus is an arbovirus within the genus Flavivirus, along with the West Nile, dengue, yellow fever, and Zika viruses. While some unknown percentage of people who are infected show no symptoms at all, the virus is fatal in approximately 10 percent of diagnosed cases, and it causes permanent neurological damage in an estimated 50 percent of those who recover. In 2017, a sixty-eight-year-old retired high school teacher from Ottawa found a feeding tick on her shoulder when she was at a cottage in southern Quebec. “I’m not a hypochondriac,” she says. Two of her friends had had a rough go with Lyme disease, so she took the tick to her doctor, who gave her a prophylactic antibiotic and—in a lucky twist—sent the tick off to Public Health Ontario for analysis. Reassured, the woman, who told me her story but doesn’t want to be “the public face of Powassan,” travelled to British Columbia on holiday.
Ten days later, in Kelowna, she developed a fever, then quickly became so ill that her partner had to drag her unresponsive body through the doors of an emergency room. Soon she was in intensive care with encephalitis and meningitis. Her children flew to her bedside because doctors warned she was unlikely to survive. Because of the known tick bite, she was treated for Lyme and tested for other tick-borne illnesses, including Powassan. But that test was negative, which isn’t uncommon: the virus may not show up in blood tests for two weeks or more. The determined—and fascinated—doctor who first saw her in the ER tracked down what Robbin Lindsay, who was eventually pulled into the case, calls the “smoking tick.” The specimen was rushed to the National Microbiology Laboratory, where it was identified as a partially engorged Ixodes marxi nymph that, when put through molecular testing, was found to contain rna for Powassan virus.
In Kelowna, the woman, still desperately ill, looked in a mirror and saw her face, frozen and twisted like that of a stroke patient. As she was being loaded onto a medevac flight back to Ottawa, she was finally told of her diagnosis, but she was too sick to care. It was only days later that she began to process that all this had come from a tick bite. She spent two months in a rehabilitation hospital, using a wheelchair, unable to feed herself; she is back to taking long walks now but has limited use of one arm, poor balance, double vision in one eye, and experiences occasional fits of choking. “People think of Lyme and think, Well, it could be treated,” she says. “But I don’t think that there’s a big awareness of the fact there are ticks that, one bite and you could die.”
The surging prevalence of Lyme disease tells us how far and how fast I. scapularis is moving. It will take Powassan virus with it, and other things too. “This tick is a microbial sponge,” Lindsay says; it seems as though anything researchers screen it for, they find. First it was Borrelia, then Anaplasma and Ehrlichia, which causes fever and muscle aches. “What’s so striking with this tick is that, the more types of pathogens you look for, the more you find.”
Tracking the diseases is one preoccupation for Lindsay and his colleagues; they also have to be on the lookout for new ticks of concern. In August 2017, a woman in New Jersey was shearing her pet sheep when she discovered ticks. And not just a few: by the time she made it to her local public health department, she had more than 1,000 ticks on her own arms and clothing. There, entomologists struggled to identify the ticks—they didn’t look like anything local—and eventually Rutgers University scientists had to use dna to establish that they were Haemaphysalis longicornis, the Asian longhorned tick. It is native to Japan, Korea, China, and far-eastern Russia. In Asia, it is a source of serious illness, including a hemorrhagic fever called Huaiyangshan banyangvirus, which is fatal for up to 30 percent of those who catch it. H. longicornis was the first invasive tick species found in the United States in eighty years, and there was hope the cold winter would kill it off. But, the following spring, the cdc reported, it was found not just in the original location but in nine more states, on wildlife, on pets, in surveillance (dragging in the woods), and on two people. Clow and Lindsay say it’s only a matter of time until it is found in Canada. Researchers can’t tell yet whether mammals or birds in North America will be receptive reservoirs for the Huaiyangshan banyangvirus (it is, however, closely related to the Heartland virus, which ticks pass to reservoirs in the US) or whether the tick can transmit pathogens to humans on this continent. For now, the biggest risk is to the livestock industry. Female Asian longhorned ticks are capable of parthenogenesis: if they don’t find a male to mate with, they simply reproduce alone. A single tick can quickly create infestations of thousands of ticks on sheep and cattle, and the effect can be so severe that the host dies of blood loss.
Every tick researcher I spoke with brought up the Asian longhorned: nobody likes these lurches into the entomological unknown. I asked Nicole Nemeth what keeps her up at night. “Just the ease with which these pathogens spread around the world, and we won’t necessarily even know it until it’s already killing either a bunch of people or a bunch of animals—that’s scary, and it could happen any moment of any day,” she said. “A tick on someone’s body could easily then drop off and bring something crazy from the other side of the world.” Crimean-Congo hemorrhagic fever, say, or Russian tick typhus.
In 2004, I was living in South Africa and travelling for work across the continent. One day I developed a terrible fever; a crusty black scab, about five centimetres in diameter, on the back of my left calf; and lymph nodes as hard as stone. A succession of doctors diagnosed me with everything from a spider bite to cutaneous anthrax to possibly leukemia before an acerbic elderly South African medic surveyed me in a hospital bed and said, “Rickettsia africae. Good old tick-bite fever.” I soon discovered that half of the people I knew in Johannesburg had had it, usually as children. In southern Africa, the bacteria is carried by Amblyomma hebraeum, a prettily patterned tick that feeds primarily on cattle. It rarely passes diseases that are fatal to humans—although the fever often lasts for weeks, as mine did—but the losses to livestock are punishing in poor countries such as Eswatini, which, I eventually figured out, is where the tick got me.
I recovered from Rickettsia africae after forty-eight hours on antibiotics (although the lymph nodes in my leg stayed rock hard for the next year). It remains, though, the sickest I’ve ever been—despite twenty-five years of reporting in countries full of all the things Nick Ogden said preoccupied him more than ticks. I never again went into long grass or paddocks in tropical countries without dousing my legs with deet.
Yet I didn’t take the same steps when I was back in Canada—not until Katie Clow took me tick dragging. She thinks about the campaigns that have, in her lifetime, persuaded people to use seatbelts, quit smoking, and wear sunscreen, and she wonders how long it will take for the change to come with ticks. “My message to people is, We are in a new era where this is part of your daily public health things that you’re supposed to be doing: if you go out in the woods, you should be checking yourself for ticks, you should be covering up.” Tuck pants into socks, wear long sleeves, apply insect repellent, and perform a tick check—behind your knees, behind your ears, and, well, where Eric Stotts would tell you to check.
Since my day in the woods with Clow, the Canadian forest trails I have walked since I was a child feel different. In the woods these days, I get the occasional cold prickle on the back of my neck. It’s not the sense that bears or wolves might be watching me. It’s not the fear of getting lost in the cold. It is the knowledge that there are thousands upon thousands of tiny hunters who can sense my breath and who are waiting, poised at the end of a long blade of grass, their front legs outstretched, for me to come close.